
Please check back, as we will continue to update these resources regularly. (Data file exchanges are referenced in the CMS, change to COB&R guidance.)Ĭlick the selection that best matches your area of interest. This document is required for PAs wishing to enter into data file exchanges with CMS to determine which of their beneficiaries are enrolled in Part D plans, in order to ensure separateness of Part D benefits and PAP assistance. The Outside the Benefit Q&A document provides further details and examples relating to CMS' policy on PAPs operating outside the Part D Benefit. Co-pay assistance is not valid where the.
MEDICARE COPAY RELIEF FULL
This overview page provides important information on CMS policy with respect to PAPs, and also provides some helpful links to other information contained on the Office of the Inspector General's Web site.įor PAPs operating outside of Part D, please review:ĬMS's Coordination of Benefits & Recovery (COB&R) guidance, linked below, provides a useful overview of CMS' policy with respect to PAPs and their interaction with Part D plans. Patients must have commercial (private) insurance, but their coverage does not cover the full cost of the prescription. Inflectra was approved by the FDA in April 2016 as a biosimilar to Janssen Biotech’s Remicade (infliximab) for.
MEDICARE COPAY RELIEF HOW TO
Find out if you’re eligible for these programs, how to apply, and other ways to save on your Medicare coverage. Pfizer announced that the Centers for Medicare and Medicaid Services (CMS) will cover the cost of the company’s biosimilar Inflectra (infliximab-dyyb) for Medicare enrollees as a Part B-covered drug. You’ll pay no more than 4.30 in 2023 for. Youll also get Extra Help paying for your prescription drugs. What to do if you get a bill You may get a bill for a small Medicaid copayment, if one applies.

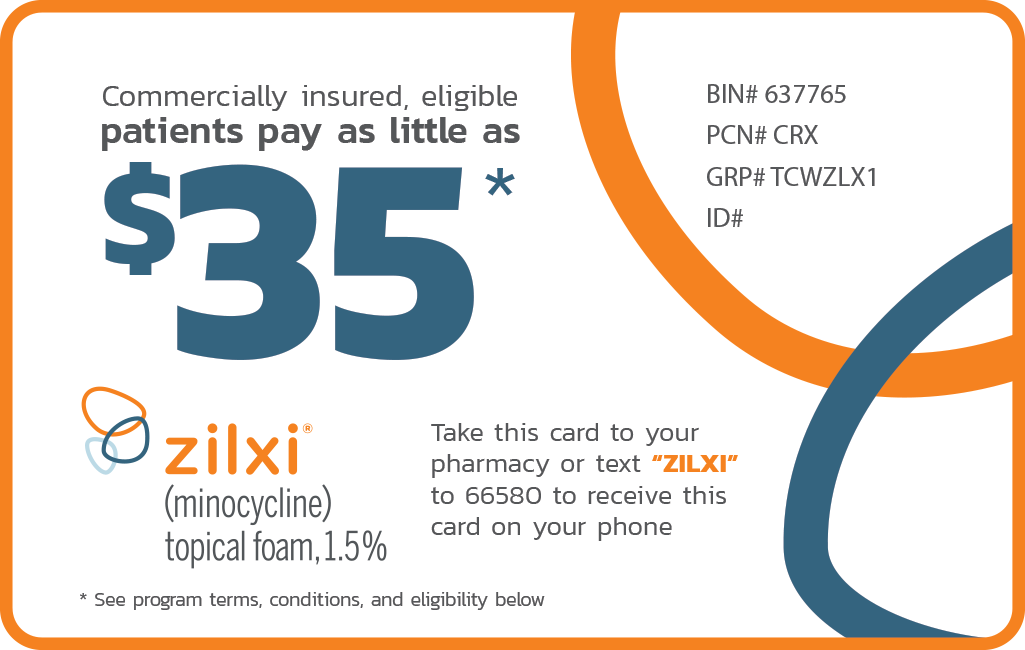
The calculation of TrOOP is important for determining whether an individual has reached the threshold for catastrophic coverage under the Part D benefit. There are programs offered through your State Medical Assistance (Medicaid) office that can help lower your Medicare costs. Medicare providers aren’t allowed to bill you for services and items Medicare covers, including deductibles, coinsurance, and copayments. The PAP's assistance on behalf of the PAP enrollee does not count towards a Part D beneficiary's true-out-of-pocket cost (TrOOP). PAPs can provide assistance to Part D enrollees and interface with Part D plans by operating "outside the Part D benefit" to ensure separateness of Part D benefits and PAP assistance. This assistance helps patients afford the out-of-pocket costs for these items that their insurance companies require. You are eligible to enroll in the Biogen Copay. The PAF Co-Pay Relief Program, one of the self-contained divisions of PAF, provides direct financial assistance to insured patients who meet certain qualifications to help them pay for the prescriptions and/or treatments they need. Pharmaceutical manufacturers may sponsor patient assistance programs (PAPs) that provide financial assistance or drug free product (through in-kind product donations) to low income individuals to augment any existing prescription drug coverage. People covered by Medicare, Medicaid, the VA/DoD, or any other federal plans are not eligible to enroll.


 0 kommentar(er)
0 kommentar(er)
